Risks and Causes of Osteoporosis in Seniors
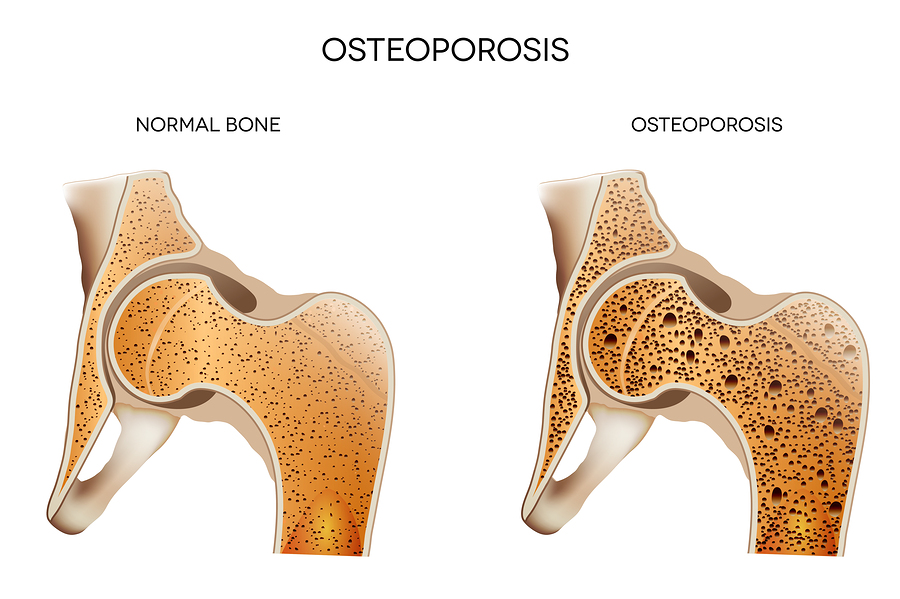
Osteoporosis is defined by low bone mass and loss of bone tissue leading to weak and fragile bones. Sometimes this includes an increased risk of fractures of the hip, spine, and wrist. It could be included in joints or all bones as well. Osteoporosis is most often recognized in older, frail women who are known to have other issues leading to this illness. With an imbalance between new bone formation and old bone resorption, the body typically is missing enough calcium and phosphate to keep a healthy bone mass. Many issues can lead to bone weakness (an easy way to think of this), and without a way to treat osteoporosis easily with drugs, it is important to manage diet and physical activity. Therefore, for your senior loved one, it is important to have senior care that can help make sure a diet is full of the proper vitamins and minerals along with enough physical activity to maintain healthy bones.
For your loved one, the introduction of senior care can help make sure that a diet full of calcium and vitamin D is brought into their daily life. A senior care member can also make sure that regular daily activity is maintained in order to keep up with bone strength and flexibility. Without senior care, your lonely loved one could more likely be alone and unhealthy, leaving them at greater risk for broken bones and other risks for osteoporosis.
The Most Likely Risks of Osteoporosis
Sometimes it may also be helpful to have senior care able to help watch for some of the most common risks of osteoporosis in your loved one’s life. Without the ability to see it on a 24-hour basis, there is an ability for senior care professionals to work with your loved one to check for the potential of osteoporosis in the long run. Some of these risks include:
- Age. Bone density peaks around age 30, with bone mass reducing afterward. After that. Therefore, strength training and weight-bearing exercises help increase bone mass, along with a healthy diet including vitamin D and calcium.
- Gender. Women are most likely to develop osteoporosis over the age of 50, four times more likely than in men. The lighter, thinner bones, smaller frames, and longer life spans of women play a part. Men also get osteoporosis, especially with a leading cause being a lack of certain hormones: estrogen in women and androgen in men. In postmenopausal women, this loss of estrogen is common, along with those facing abnormal or absence of menstrual periods.
- Family history. Having a parent or grandparent with osteoporosis is a risk factor as well. Even if a family member had symptoms of osteoporosis, like a fracture after a minor fall, it could be a risk.
- Bone structure and body weight. Petite, thin women face a greater risk chance of developing osteoporosis. One reason is that they have less bone to lose than women with more body weight and larger frames. Similarly, small-boned, thin men are at greater risk than men with larger frames and more bodyweight.
- Broken bones and diseases. If you’ve had fractures before, your bones may not be as strong. Some diseases such as rheumatoid arthritis raise the odds that you’ll get osteoporosis. Rheumatoid arthritis itself is a risk factor for osteoporosis. Other conditions that may lead to osteoporosis include overuse of corticosteroids (Cushing syndrome), thyroid problems, lack of muscle use, bone cancer, certain genetic disorders, use of certain medications, and problems such as low calcium in the diet.
- Ethnicity. Research shows that Caucasian and Asian women are more likely to develop osteoporosis than women of other ethnic backgrounds, with hip fractures twice as likely to happen in Caucasian women.
- Some medications. Certain prescription medications (e.g. prednisone) also boost the risk of getting osteoporosis.
Things to Avoid When Facing a Risk of Osteoporosis
While there are many uncontrollable factors that may contribute to your osteoporosis risk, there are certain lifestyle behaviors that you control to also impact your chances of developing the disease:
- Eating a diet low in calcium and vitamin D. A diet rich in calcium and vitamin D is important to increase and sustain healthy bone growth. Calcium promotes healthy bones and vitamin D helps the body effectively absorb calcium. Foods high in sodium cause calcium loss, leading to bone loss.
- Being inactive. Exercise helps ward off osteoporosis by strengthening your bones, just as it strengthens your muscles. Strong bones are less likely to fracture.
- Smoking. It’s bad for your bones, so work with your doctor to kick this habit ASAP. Cigarette smoking plays a negative effect on other efforts played to improve your senior’s health, so it is important to quit if a risk for osteoporosis has been identified.
- Alcohol. Heavy drinking also leads to thinning of the bones and makes fractures more likely. Limit alcohol intake to two drinks a day or less.
- Caffeine found in coffee, tea, and soda decreases calcium absorption and leads to bone loss.
- Soft drinks. The caffeine and phosphorus found in colas may contribute to bone loss. It is not clear if the link to bone loss is because people choose soft drinks over milk and other calcium-containing beverages, or if cola directly causes bone loss.
Many foods help prevent osteoporosis. A number of scientific studies have shown that eating more fruits and vegetables leads to stronger bones. Low-fat dairy products are high in calcium, and many are fortified with vitamin D and help strengthen bones. Fatty fish such as salmon, mackerel, tuna, and sardines are high in vitamin D. Canned sardines and salmon (with bones) are high in calcium.
If you or an aging loved-one is considering Senior Care in El Segundo, CA please contact the caring staff at American Geriatric Care Management, LLC today at (310) 648-0614.
Sources:
https://www.premierformulas.com/the-ultimate-guide-to-healing-osteoporosis-naturally/
- 4 Things You Must Do to Prepare your Elderly Loved Ones for 4th of July Fireworks - July 1, 2020
- Types of Incontinence Your Loved One Might Have - March 22, 2020
- An Update Regarding Coronavirus (COVID-19) - March 22, 2020
